Hey there, friend. Imagine this: You’re bending down to pick up your kid’s toy, or maybe just twisting to grab something from the back seat of your car, and suddenly—bam—a jolt of pain hits your lower back like a lightning bolt. It doesn’t stop there; it radiates down your leg, making every step feel like a chore. If that sounds familiar, you might be dealing with herniated disc symptoms, that sneaky spinal issue that catches so many of us off guard. I’ve been there myself, years ago after a weekend of heavy yard work, wondering if I’d ever move without wincing again. It’s scary, right? But here’s the good news: Most folks get through it, and knowing what you’re up against can make all the difference.
Herniated disc symptoms aren’t just about pain—they’re a signal from your body that something in your spine needs attention. Whether it’s numbness in your toes or a weakness that makes holding a coffee mug tricky, these signs can mess with your energy, your mood, and your plans. But you’re not alone; millions deal with this every year, and with some smart, gentle strategies, you can ease the discomfort and get back to what matters. In this post, we’ll walk through it all together, like chatting over coffee, sharing stories, facts, and tips that actually help without overwhelming you.
Think of this as your compassionate guide—no medical jargon overload, just honest insights to help you feel empowered. We’ll cover what these symptoms really feel like, why they happen, and practical ways to cope, drawing from reliable sources and real-life examples. By the end, you’ll have a clearer path forward, because everyone deserves to live without that nagging ache holding them back.
Key Takeaways
- Herniated disc symptoms often include sharp pain, numbness, or weakness that radiates from your back to your limbs, but they vary by location in the spine.
- Most cases stem from everyday wear and tear or poor lifting habits, and they’re more common in folks aged 30-50, affecting about 1-3% of adults symptomatically.
- Good news: Around 90% of people improve within 4-6 weeks with rest, meds, and simple lifestyle tweaks—no surgery needed for most.
- Prevention is key: Focus on core strength, proper posture, and maintaining a healthy weight to keep your spine happy long-term.
- If symptoms worsen or include loss of bladder control, see a doctor ASAP—it’s rare but serious.
Understanding the Basics of a Herniated Disc
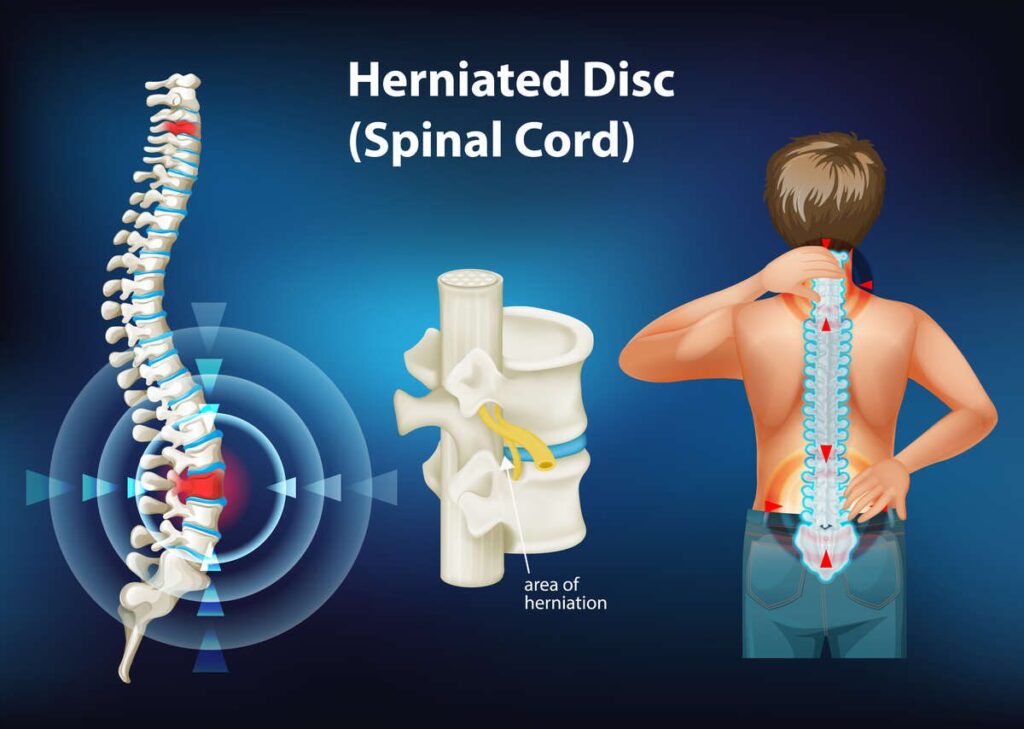
Let’s start simple, because when herniated disc symptoms hit, it can feel like your body’s betraying you. Picture your spine as a stack of cushy donuts—these are your discs, soft and jelly-like in the middle, with a tougher outer ring. They act as shock absorbers between your vertebrae, keeping everything flexible and pain-free. But sometimes, that outer ring cracks or tears, and the inner gel pushes out. That’s a herniated disc, also called a slipped or bulging disc. It doesn’t always hurt, but when it presses on nearby nerves, ouch—that’s where the trouble starts.
I remember talking to my neighbor, Mike, a 45-year-old teacher who loves hiking. One day, he twisted funny while reaching for a book on a high shelf, and boom—his lower back screamed. He described it as a deep ache that turned into shooting pain down his leg. Turns out, it was a classic lumbar herniated disc, the most common type, happening in the lower back where we put the most stress. Up in the neck? That’s cervical, and it might zap your arms instead. Either way, it’s your body’s way of saying, “Hey, slow down and listen.”
Why does this matter? Because recognizing herniated disc symptoms early can prevent them from snowballing. According to experts, more than 3 million Americans deal with this annually, making it a top cause of back and leg pain. It’s not just about age; even young adults in their 20s can have silent disc issues, with studies showing up to 30% having protrusions without a clue. So if you’re feeling that twinge, don’t brush it off—it’s common, but addressable.
What Herniated Disc Symptoms Actually Feel Like
Okay, let’s get real about the sensations, because herniated disc symptoms aren’t one-size-fits-all. For many, it starts subtle—a dull ache in your lower back after a long day. But then it ramps up. Take Jen, a 38-year-old mom and office worker I know. She woke up one morning with what she thought was a pulled muscle, but by afternoon, a sharp, burning pain shot from her buttock down her thigh. “It felt like an electric shock every time I moved,” she told me. That’s sciatica, a hallmark of lower back herniations, where the disc irritates the sciatic nerve.
Numbness and tingling? Yeah, those creep in too, like pins and needles in your calf or foot. It’s unnerving, making you wonder if your leg’s falling asleep permanently. And weakness—oh, that’s sneaky. You might drop things more often or stumble while walking, as the affected muscles lose their oomph. In the neck, symptoms mirror this but upstairs: shoulder pain that radiates to your fingers, maybe even headaches if it’s bad.
Rhetorically, have you ever felt that? A pain so targeted it makes you question every twist and turn? It’s exhausting, emotionally too. But here’s a gentle insight: These feelings are your nerves talking, not a life sentence. Symptoms often hit one side of the body, and they worsen with coughing, sneezing, or sitting too long. If it’s mild, it might just be a nagging discomfort; severe cases? Debilitating. The key is tuning in without panic—most fade with time.
Real-Life Feels: Stories from Everyday Folks
To make this hit home, consider Tom, a 52-year-old mechanic. His job involves lots of bending, and one heavy lift led to instant leg weakness. “I couldn’t trust my foot on the brake,” he shared. After tests, it was a herniated disc compressing a nerve. Or Sarah, 29, a runner who ignored early tingling until it turned into full-blown numbness during a jog. These micro-anecdotes show it’s not just “old people stuff”—it hits active lives hard.
Stats back this up: Men are twice as likely to experience it, often between 30 and 50, when life’s demands peak. Worldwide, about 5.5% of folks have symptomatic disc issues, that’s over 400 million people. So if you’re nodding along, know you’re in good company.
Why Do Herniated Discs Happen to Good People?
Life’s not fair sometimes, is it? Herniated disc symptoms often sneak up because of gradual wear—disk degeneration from aging makes them less bouncy, more prone to tears. But it’s not just time; everyday habits play a huge role. Lifting wrong, like using your back instead of legs, is a biggie. I learned that the hard way after hauling boxes during a move. Twist while lifting? Double trouble.
Other culprits: Excess weight adds pressure, like carrying an extra backpack on your spine daily. Smoking? It starves discs of oxygen, speeding breakdown. Jobs with repetitive motions—think construction or desk work with poor posture—up the risk. Even genetics: If your family has back woes, you might too. And trauma, like a fall or car accident, can trigger it instantly.
Sedentary lifestyles don’t help either. Sitting for hours vibrates your spine subtly, wearing it down. Frequent drivers, beware—that engine hum isn’t innocent. But here’s the emotional honesty: Blaming yourself isn’t useful. It’s often a mix of factors, and understanding them empowers change, not guilt.
Risk Factors You Can Actually Influence
Sure, you can’t change your genes, but weight? Posture? Absolutely. Carrying extra pounds stresses lower back discs, increasing herniation odds. A study notes obesity as a key player. And smoking—quitting could be your spine’s best friend. Physically demanding jobs amplify risks, but even office warriors suffer from slouching.
One quote that sticks: “Your spine is only as young as it feels,” from a physical therapist I chatted with. Small shifts, like standing breaks, can rewrite your story.
When Herniated Disc Symptoms Mean It’s Time for Help
Not every ache needs a doctor, but ignoring herniated disc symptoms can backfire—literally. If pain travels down your arm or leg, or comes with numbness that lingers, flag it. Weakness making daily tasks tough? Same. And red flags: Bladder or bowel issues, like sudden incontinence, scream emergency—it’s rare cauda equina syndrome, needing quick action to avoid permanent damage.
Saddle anesthesia, that numb feeling in your inner thighs or groin? Don’t wait. Worsening symptoms despite rest? Time to chat with a pro. They’ll do a physical exam—testing reflexes, strength, sensation—and maybe imaging like an MRI to confirm. It’s not scary; it’s clarifying.
For peace of mind, start with your primary doc or a spine specialist. Early intervention often means simpler fixes.
Everyday Strategies to Ease Herniated Disc Pain
Alright, let’s talk relief—because dealing with herniated disc symptoms doesn’t mean suffering in silence. First up: Rest, but smart rest. A day or two off your feet if it’s bad, but don’t lounge for weeks; that stiffens muscles. Alternate ice and heat: Ice numbs pain first 48 hours, heat relaxes after.
Over-the-counter helpers like ibuprofen cut inflammation, easing that burn. But listen to your body—if it flares, ease up. Gentle walks keep blood flowing without strain. Jen swore by propping her legs up while reading, reducing nerve pressure.
Posture tweaks: Sit with support, stand tall. Avoid slouching like the plague. And lifting? Bend at knees, hug loads close. These aren’t chores; they’re kindness to your spine.
Natural Remedies and Mind-Body Hacks
Ever tried mindfulness for pain? It sounds woo-woo, but breathing deep during flares calms the nervous system. A friend used apps for guided meditation, noticing less intensity. Or acupuncture—some find it eases symptoms, though evidence varies.
Hydration and nutrition matter too. Water keeps discs plump; anti-inflammatory foods like salmon or berries support healing. No miracles, but they stack the deck in your favor.
Exercises and Stretches That Can Make a Difference
Movement is medicine for herniated disc symptoms, but gentle is key. Start with physical therapy— a pro can tailor it. Basic ones: Cat-cow pose for flexibility, or child’s pose to stretch the back softly.
For lower back: Knee-to-chest pulls, holding 20 seconds. Bridge poses build core strength, stabilizing your spine. Aim for 10-15 minutes daily, stopping if pain spikes.
Neck issues? Chin tucks or shoulder rolls. Remember Mike? PT helped him hike again in months. Experts recommend trunk-strengthening to support the spine. It’s about building resilience, not pushing through pain.
A Sample Gentle Routine
- Warm-up: March in place, 2 minutes.
- Stretch: Hamstring pulls, seated.
- Strengthen: Planks, modified on knees.
- Cool down: Deep breaths.
Consistency wins—start slow, celebrate progress.
Medical Treatments: When Home Care Isn’t Enough
If herniated disc symptoms persist past a month, docs might suggest more. Cortisone injections zap inflammation around nerves, offering weeks of relief. Muscle relaxers for spasms, or short-term opioids if severe—but sparingly.
Surgery? Rare, for 10% or so. Microdiscectomy removes the offending bit, minimally invasive with quick recovery. It’s not first-line; most heal naturally.
Weigh pros/cons with your doc—it’s your body, your call.
Preventing Herniated Discs Before They Strike
Why wait for symptoms? Prevention feels empowering. Core exercises like Pilates fortify your back. Maintain weight—every pound off eases spinal load.
Posture: Ergonomic setups at work, breaks to stretch. Quit smoking for better disc health. And exercise regularly—mix cardio, strength, flexibility.
One tip: Mindful movement. Before lifting, think “legs, not back.” It becomes habit, sparing future pain.
Habits from Those Who’ve Been There
Tom now warms up before work; Sarah mixes yoga with runs. Small changes, big impact.
Living Day-to-Day with Herniated Disc Symptoms
It’s not just physical—herniated disc symptoms can drain you emotionally. Frustration from canceled plans, worry about recurrence. But many thrive. Adapt: Use tools like lumbar cushions, delegate heavy tasks.
Support matters—talk to friends, join online groups. One woman shared, “It taught me patience with my body.” Ups and downs, but resilience grows.
Stats show good outlook: Most back to normal in weeks. You’re tougher than you think.
Final Thoughts
Whew, we’ve covered a lot, from that initial zap of herniated disc symptoms to ways to bounce back stronger. Remember, this isn’t about perfection—it’s about listening to your body with kindness, making tweaks that fit your life. You’ve got the tools now: Awareness of symptoms, prevention habits, and when to seek help. Most importantly, know that healing happens, often on its own timeline.
If there’s one small action to take today, try a gentle stretch or a short walk. Feel the difference? Keep going—you deserve to move freely and joyfully. For more insights on health and wellness, explore other posts on Upvolta.com. You’ve got this, friend.
For trusted resources, check out these:
- Mayo Clinic on Herniated Disks
- Cleveland Clinic’s Guide to Herniated Disks
- Johns Hopkins Medicine on Lumbar Disc Disease
- AAOS on Herniated Disk in the Lower Back
FAQ
What are the most common herniated disc symptoms?
Sharp pain radiating to arms or legs, numbness, tingling, and muscle weakness are typical, often worse with movement.
Can herniated disc symptoms go away on their own?
Yes, most do within 4-6 weeks with rest and conservative care, as the body reabsorbs the herniated material.
How do I know if my back pain is from a herniated disc?
If it shoots down a limb and includes numbness or weakness, it might be—see a doctor for confirmation via exam or imaging.
Are herniated disc symptoms worse in the morning?
Often yes, due to overnight fluid buildup in discs, but gentle movement can ease it.
What should I avoid with herniated disc symptoms?
Heavy lifting, twisting, prolonged sitting, and high-impact activities until symptoms improve.
Can exercise help herniated disc symptoms?
Absolutely, low-impact ones like walking or core strengthening, but start under guidance to avoid aggravation.
Is surgery always needed for herniated discs?
No, only about 10% need it if symptoms persist or cause severe issues like nerve damage.
How can I prevent herniated disc symptoms from returning?
Build core strength, maintain good posture, stay at a healthy weight, and lift properly.
Do herniated disc symptoms affect sleep?
They can, with pain flaring at night—try side-sleeping with a pillow between knees for relief.
Are there home remedies for herniated disc symptoms?
Ice/heat therapy, over-the-counter pain relievers, and gentle stretches can help, but consult a pro if persistent.